Macular Degeneration
Age-related macular degeneration (ARMD) is a disease that affects older patients. ARMD is the leading cause of visual impairment and blindness in Americans over the age of 60. It affects more than two million people. For as yet unknown reasons, the center of the retina, the macula, begins to deteriorate with time. Because the macula is responsible for virtually all of a person’s sharp, central vision, any degeneration can lead to significant deficits. There are two defined types of macular degeneration.
Dry ARMD
Approximately 90% of AMD cases are the dry form, which causes a gradual vision loss due to aging of the macula. In the dry form, there is loss of central macular tissue. There is no know etiology, but the disease only occurs in older individuals. Some researchers believe that age-related oxidative damage may be part of the cause. From several major national and international studies, there is strong evidence that a diet high in anti-oxidants reduces the risk of progression of macular degeneration. It is not a cure, nor can it reverse any damage that has occurred.
In 2006, the first Age-Related Eye Disease Study (AREDS) led by the National Institutes of Health found that patients taking the original AREDS supplement formulation — 500 mg of vitamin C, 400 IU of vitamin E, 80 mg of zinc, 15 mg of beta-carotene, and 2 mg of copper — were 25% less likely to progress to advanced AMD than patients who received a placebo. There was additional evidence outside of the trial that suggested that diets high in lutein, zeaxanthin, and omega-3 fatty acids might reduce progression of AMD. For this reason, a second large multi-center trial was commenced, named AREDS2. Other research suggested that beta-carotene, which was part of the original AREDS formula, might increase the risk of lung cancer in smokers, so it needed to be studied more carefully. The dosage of zinc also was examined in AREDS2. There was concern that the 80-mg dose of zinc in the original study might place some patients at risks of side effects.
In 2013, the AREDS2 Study Group released their first conclusions. Although the study design was complex, essentially AREDS2 discovered that those who took an AREDS formula with lutein and zeaxanthin but no beta-carotene, reduced their risk of AMD progression by about 20%, compared with participants who took an AREDS formulation with beta-carotene but no lutein or zeaxanthin. This particular sub-group’s results were especially notable, because the removal of beta-carotene from the recommended AREDS formula would also reduce the potential for increased lung cancer risk in previous or current smokers with AMD. Since the release of the AREDS2 data, Dr. Liu’s recommendations for AREDS vitamin supplements are as follows:
- No evidence of AMD on examination: Dr. Liu recommends a diet rich in green, leafy vegetables and omega-3 fatty acids, supplemented with a daily multivitamin.
- Evidence of early or moderate AMD on exam: Dr. Liu recommends the same healthy diet and multivitamin, supplemented with an AREDS2 formula vitamin containing lutein and zeaxanthin.
- Evidence of advanced AMD on exam: Dr. Liu does not recommend adding an AREDS vitamin, because this has not been shown to prevent progression in either of the AREDS studies.
Wet ARMD
Around 10% of ARMD cases are known as the wet form. This form can progress quickly, resulting in blurring and potential loss of central vision. Nearly 200,000 people are diagnosed with wet ARMD each year. The pathophysiology involves the growth of abnormal blood vessels in the back of the eye. As the blood vessels grow, they can leak blood and fluid, which damage the macula. In addition to the abnormal growth of blood vessels, certain proteins are thought to play a major role in causing wet ARMD.
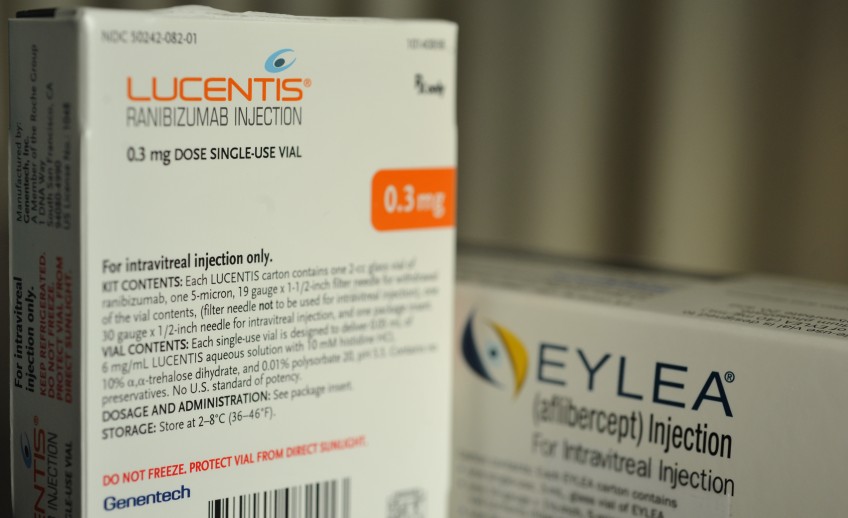
Although there is no cure, there is a treatment to arrest and potentially reverse the effects of wet ARMD. Intravitreal injections are used for the treatment of the abnormal blood vessels that grow underneath the retina in this condition. A number of medicines are now indicated for this condition, including Avastin, Lucentis, Eylea, and steroids. These are known as anti-VEGFs for their mechanism of action (they are inhibitors of vascular endothelial growth factor, a protein which is involved in the proliferation of abnormal blood vessels). When it was introduced, Lucentis became a breakthrough treatment for wet ARMD. Not only did some patients stabilize, some actually improved their vision through serial treatment. These medicines are a treatment that targets these proteins–preventing them from causing more damage and possibly even reversing their effects. In key clinical trials, about 95% of patients treated with Lucentis found that their vision stayed the same (vision loss did not progress) and up to 40% of those patients found that their vision significantly improved. However, wet ARMD is a chronic condition. In many cases, it can be managed and potentially controlled with anti-VEGF treatments. Call for an appointment with Dr. Samuel Liu if you or a loved one is concerned with macular degeneration.